Our first piece focuses on the dynamic between productivity and speed. Jack explained that throughout his extensive range of experiences, this tension has remained a common thread.
The need for speed
Imagine the scene. It’s a typical workday for Jack and his team. The call queue is buzzing. Members are on hold, waiting to speak to someone about the most critical and personal of issues – their healthcare. Many of them are in distress. Perhaps they are angry about a change of policy. Maybe they are sick, or deeply concerned about a loved one. Jack’s busy customer service teams are working tirelessly to meet members’ demands, getting through as many calls as possible. They handle thousands, or even tens of thousands, of transactions each day. It’s a high stake, fast-paced environment.
Every day, senior managers face the same challenges. Making the cogs turn more smoothly. Shaving off inefficiencies. Always thinking of the bottom line. Jack told us:
“The emphasis on speed permeates all the operational areas. The variable within different organizations is how much quality is also a factor in how you work. In my opinion, you need both. You need to move quickly, but you need to be able to deliver a really good quality experience. There’s probably a disproportionate focus on speed.”
The call center quandary…
And what if the call center volume creeps up even further? The leadership team have two options: squeeze staff, or compress demand. Most senior managers will consider:
- Hiring more staff
- Making current staff more productive. Reduce talk time. Increase the number of calls per day. Essentially, overworking their employees.
But Jack champions a different approach. He argues for compressing demand on why people are calling. And that requires a focus on quality right from the start of the member’s journey.
The quality approach
Just consider why people call their healthcare insurance providers. Perhaps a letter has fallen onto their doorstep, and they don’t understand it. This happens regularly. Last year, we carried out research into the readability of Medicare information. We discovered that 86.6% of insurers are not communicating effectively with those aged 65 and older. Insurers pitched their communications, on average, at a grade level of 7.4. For reference, the recommended grade level for optimum readability amongst this cohort is grade 6.
And Jack has seen this happen time and time again. Often, communications are written by a team of people who have no writing skills whatsoever. A claims or service team, for example. The result is a communication created without a thought for member/customer experience. Or how members will actually interact with it. As Jack says:
“You get very poorly constructed letters, you have grammar issues. You have punctuation issues, you have formatting issues. And, most importantly, you have clarity issues.”
So what does the member receiving the letter do? She panics and gets on the phone.
And the most frustrating part of this story is that this member’s claims questions would be so easy to address if only a holistic approach had been taken towards member communication. If insurers invested enough thought and time in crafting the right message, in the correct way. The member would then have a better chance of understanding its meaning and feel reassured. And what if she still had questions? She could be directed to a FAQ page online, perhaps.
A win-win solution for company and member
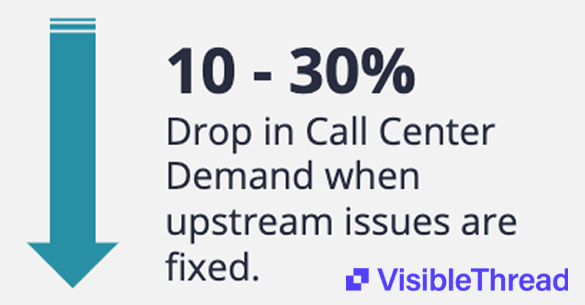
If members with easy-to-answer questions find their answers elsewhere, the call center load reduces. Jack estimates that demand on the call center can drop 10-30% if you fix upstream issues. You’re left with the folks who really need to talk to someone. These members make up the small percentage who have very complicated issues. In the “speed” model, they might call back up to fifteen times. But because these staff are highly skilled and expertly trained, members are now more likely to get their issues resolved first time. The first touch resolution model is the most economical, and it’s also the best option for the individual.
And not only that. Because the calls have been compressed, there’s a direct impact on recruitment, training and retention of staff. The company needs fewer people working the call queue, but these employees must be highly skilled. Because these cases are complex. The “higher quality” employees demand a higher salary per individual, but there are fewer of them. Another saving for your bottom line.
And finally, this approach also makes for happier members. She is now more likely to pitch your service to HR when insurance renewals come around. There’s a positive impact on renewals, retention, and acquisition. As well as member experience, of course.
Switching focus from speed to quality
So how is this done? How does an organization switch from a machine of mass recruitment, mass training, mass call volume, to a company in which quality is king? Jack argues that the following steps would be a great place to start:
1. Onboarding for all members
Think about the member’s journey, right from enrollment. Does she get a pack of information sent out? Or a courtesy call to welcome her to the service, and offer answers to any initial questions? Health is highly emotional. If an organization invests in a member upfront, they build that member’s trust in the service.
2. Keep track of all communications
How do you ensure that all customer content is easy to consume? Multiple teams and departments now create communications. It’s a struggle for any organization to manage this at scale. But using a solution such as VT Insights, a company can easily keep track of the readability of all online and offline content. The solution flags:
- Jargon – a big issue in healthcare
- The use of long sentences
- Overuse of the passive voice
- Grade level
It doesn’t matter which teams are writing content, VT Writer allows all employees to easily score their own writing. And using VT insights, management can also keep track of outgoing content, ensuring it all achieves a minimum standard of readability.
3. Make sure answers to the “easy to resolve” questions are accessible
Jack’s best advice? Make it easy on the member. There’s a reason that Amazon achieves record growth, year on year. They prioritize customer experience, and the issues that customers care about the most. Fast delivery, excellent service. Your healthcare member also needs to know that everything is taken care of. And that he can easily find answers to his questions.
Progress comes from the top
With major benefits on offer, it is surprising that more health insurers haven’t jumped on the quality bandwagon. In Jack’s words:
“I’ve worked at a lot of places. I’ve not seen one place that puts the proper focus on quality.”
According to Jack, leadership teams really need to embrace a different way of working. He says that “Senior management plays a critical role in the philosophy of how the call center is run.” They need to step back and assess what’s happening as a whole. Of course, productivity will always play a crucial role in the world of a call center. But, in Jack’s words, “you have to focus on quality equally, if not more.”
And for those who decide to embrace this model, there are huge opportunities. Focus on quality. Offer a superior member experience. Boost your bottom line.